Engineering Surgical Equipment
This project explores how current surgical equipment can be improved from an engineering point of view. The selected medical field for this particular project is obstetrics and gynecology. Obstetrics is a surgical specialty associated with the care of a woman and her offspring during pregnancy, childbirth, and puerperium. Gynecology is the specialty of diseases of the female reproductive system. Certain medical devices may be used to ease the mother during labor and delivery. Regardless of the method of delivery, fetal heart rate should be monitored closely. Scroll to read more about what improvements can be made on fetal heart rate monitors.
There are two methods of delivering a baby. The first method is natural birth, in which the baby moves through the birth canal. This method consists of three stages: Cervix dilation, pushing and birth, and the delivery of the placenta. The first stage can then be divided into three sub-stages: early labor, active labor, and transition. Early labor ranges from 8-12 hours with 30 to 45-second contractions and 5 to 30 minutes in between each contraction. The cervix effaces and dilates 3 cm. During this period, the mother may have mixed emotions and anticipation, therefore it would be the best if she rests at home and drink plenty of fluids. As contractions become more frequent, the mother slowly progresses towards active labor. During this stage, the mother should start proceeding to the hospital or birthing center, as her cervix dilates to 7 cm. Contractions are 45-60 seconds long, with 3 to 5 minute in between each contraction. This is when the baby moves down in the mother’s pelvis and faces back. Due to the increased intensity, active labor is shorter than early labor and lasts from 3 to 5 hours. The last sub-stage is the transition stage. This is when the cervix dilates to 10 cm with 60 to 90-second contractions and 3 minutes between each contraction. The mother may experience hot flash, sudden chill, nausea, vomiting, and may also be overwhelmed and disoriented during this 30-min to 2-hour stage. When the cervix is completely dilated to 10 cm, the mother arrives at the second stage and starts pushing the baby out of her uterus. This may last from 20 minutes to 3 hours. The mother continues to experience 45 to 90-second contractions during this stage, with a 3 to 5-minute rests between each contraction. Once the baby is born, the mother arrives at the third stage, or delivery of the placenta. Due to a sudden shrinking of the uterus, the placenta detaches itself and is pushed out of the uterus. The total labor time may last from 6 to 24 hours.
The second method is Cesarean section, or the doctor surgically delivers the baby by making incisions on the mother’s abdomen. This method of delivery is generally used when the mother experiences dystocia, or prolonged labor. Other factors that may result in Cesarean section delivery are cephalopelvic disproportion (CPD), or the baby’s head is too large for the mother’s pelvis, breech position, fetal distress, placenta becomes detached, prolapsed umbilical cord, and uterine rupture. Generally, Cesarean sections are less problematic, because there are less special cases and standard procedures and operations are followed. However, C-section may require the mother to be hospitalized for a few days after child birth.
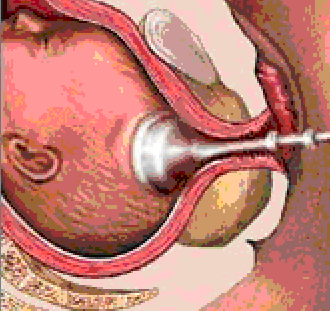
In either method of childbirth, fetal heart rate must be present to detect any unusual heart rate of the fetus or fetal distress. Such a device is known as the fetal heart monitor, which utilizes ultrasound waves to detect fetal heart and translating the changes in the waves to sound. These monitors can also create a visual record of the fetal heart rate by instantaneous calculations of the heart rate. There are two methods used in this process: external monitoring and internal monitoring. To measure fetal heart rate externally, a strap of an ultrasound transducer is strapped over the mother’s abdomen and picks up baby’s heart beat. This method is commonly used for prenatal visits. Fetal heart monitors provides the mother and the doctor with information about the baby’s well-being, health condition, especially during the last trimester of pregnancy. It is also used to determine to assess how well the fetus is doing as the baby tolerates the stresses of labor. Therefore it is important that the baby’s heart rate is monitored during birth, and so a second method, or internal monitoring, may be utilized to determine fetal heart rate while the mother is in labor. This method would require the mother’s cervix to be dilated, and that the mother’s “water has broken”. A small clip is placed on the baby’s scalp, which directly measures the baby’s heart rate.
During labor, certain medical devices may be used to help ease the process. When the doctor observes a prolonged labor, he/she may assist the mother with forceps or manual vacuum extractors, given the mother and fetal conditions. A vacuum extractor is a simple manually operated pump that generates a negative force at the end of the suction cup. As mentioned above, it is critical that fetal heart rate is continuously monitored until the baby is fully delivered. Current medical devices use separate instruments to perform single tasks. However, after examining the geometries of a vacuum extractor and internal fetal heart rate monitors to be similar, it may be useful if one single device can do both jobs. A vacuum extractor consists of a funnel-like shape that covers the scalp of the baby.